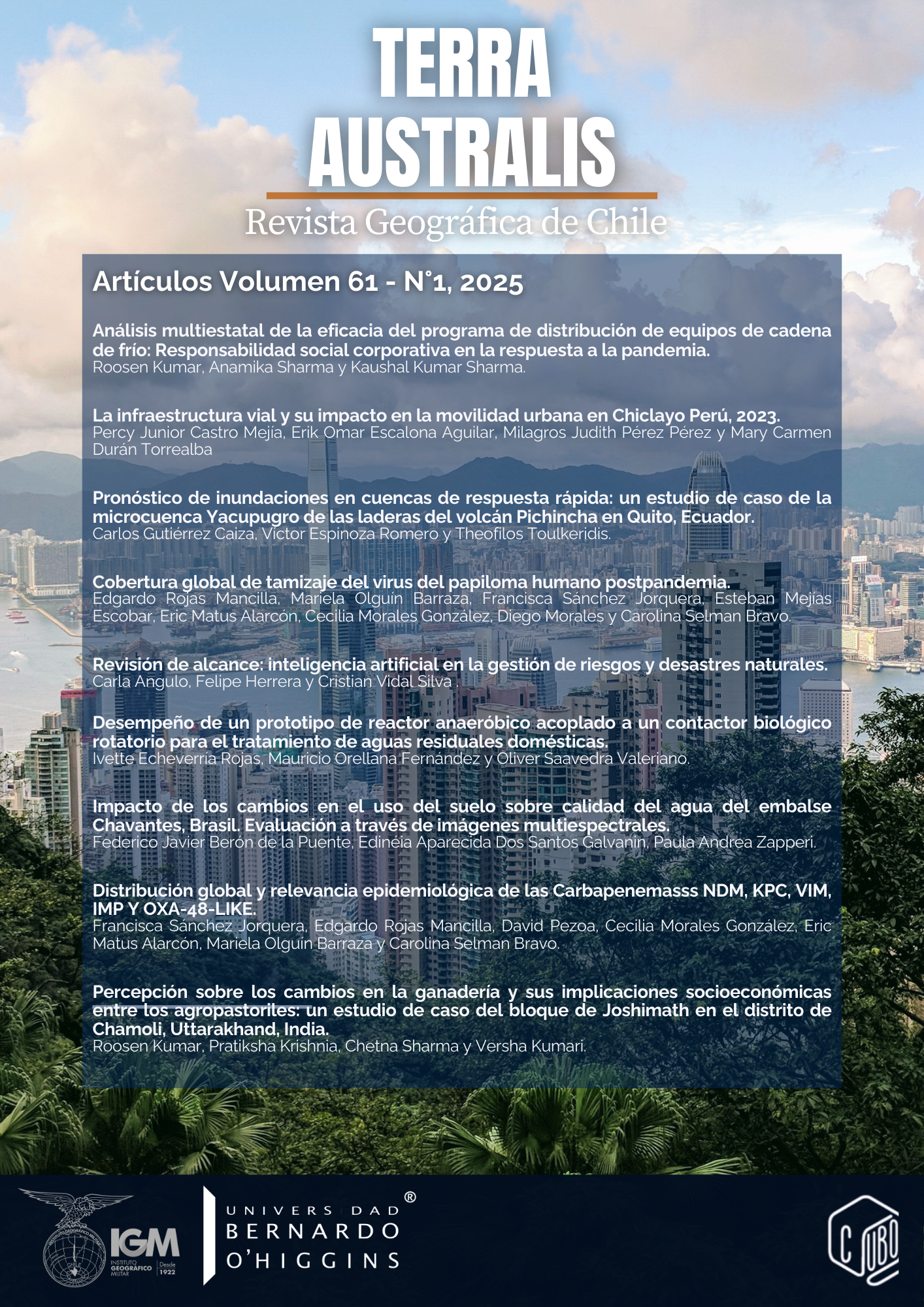
Global distribution and epidemiological relevance of NDM, KPC, VIM, IMP AND OXA-48-like Carbapenemases
DOI:
https://doi.org/10.23854/07199562.2025611.sanchezKeywords:
Carbapenemases, antimicrobialresistance, multidrug-resistant bacteria, epidemiologicalsurveillanceAbstract
Carbapenemase-mediated resistance, driven by enzymes that inactivate last resort carbapenem antibiotics, has emerged as a critical global health threat. To delineate its true scope, we conducted an exhaustive review of the past five years’ literature, focusing on the five principal carbapenemases (KPC, NDM, VIM, IMP, and OXA-48-like) in human clinical isolates. All relevant studies were synthesized into a unified database, which served as the basis for generating individual world maps for each enzyme and a composite map illustrating their co-occurrence. These visual tools illuminate the uneven yet interconnected nature of carbapenemase dissemination, underscoring the value of spatially resolved data in combating antimicrobial resistance. Our findings reveal distinct regional patterns: KPC dominates much of the Americas and Western Europe; NDM is most burdensome in the Indian subcontinent and North Africa; VIM remains concentrated in Southern Europe; IMP is endemic in Japan and parts of China; and OXA-48-like enzymes prevail around the Mediterranean and in the Middle East. These disparities reflect local genetic transfer dynamics, via plasmids, integrons, and other mobile elements, as well as variations in antibiotic use practices and surveillance capacity. Accurate, up-to-date distribution maps are therefore indispensable for tailoring surveillance strategies, optimizing antimicrobial stewardship, and directing research funding, all of which are vital for slowing the spread of these formidable resistance determinants.
Downloads
References
Alvisi, G., Curtoni, A., Fonnesu, R., Piazza, A., Signoretto, C., Piccinini, G., Sassera, D., &Gaibani, P. (2025). Epidemiology and Genetic Traits of Carbapenemase-Producing Enterobacterales: A Global Threat to Human Health. Antibiotics (Basel, Switzerland), 14(2), 141. https://doi.org/10.3390/antibiotics14020141
Ambler R. P. (1980). The structure of beta-lactamases. Philosophical transactions of the Royal Society of London. Series B, Biological sciences, 289(1036), 321–331. https://doi.org/10.1098/rstb.1980.0049
Aminov R. I. (2009). The role of antibiotics and antibiotic resistance in nature. Environmentalmicrobiology, 11(12), 2970–2988. https://doi.org/10.1111/j.1462-2920.2009.01972.x
Andrade, L. N., Curiao, T., Ferreira, J. C., Longo, J. M., Clímaco, E. C., Martinez, R., Bellissimo-Rodrigues, F., Basile-Filho, A., Evaristo, M. A., Del Peloso, P. F., Ribeiro, V. B., Barth, A. L., Paula, M. C., Baquero, F., Cantón, R., Darini, A. L., & Coque, T. M. (2011). Dissemination of blaKPC-2 by the spread of Klebsiella pneumoniae clonal complex 258 clones (ST258, ST11, ST437) and plasmids (IncFII, IncN, IncL/M) among Enterobacteriaceae species in Brazil. Antimicrobialagents and chemotherapy, 55(7), 3579–3583. https://doi.org/10.1128/AAC.01783-10
Antequera M, A., Sáez B, C., Ciudad S, M., García B, M. J., Moyano V, B., Rodríguez C, P., Roy V, E., Aguilera G, M., Alonso N, E., Cárdenas I, M. J., Castro G, S., Domingo G, D., & Barrios B, A. (2020). Epidemiología, tratamiento y mortalidad en pacientes infectados por enterobacterias productoras de carbapenemasas: estudio retrospectivo [Epidemiology, treatment and mortality in infectionbycarbapenemase-producingEnterobacteriaceae: retrospective study]. Revista Chilena de Infectologia, 37(3), 295–303. https://doi.org/10.4067/s0716-10182020000300295
AntimicrobialResistanceCollaborators (2022). Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet (London, England), 399(10325), 629–655. https://doi.org/10.1016/S0140-6736(21)02724-0
Armstrong, T., Fenn, S. J., & Hardie, K. R. (2021). JMM Profile: Carbapenems: a broad-spectrum antibiotic. Journal of medical microbiology, 70(12), 001462. https://doi.org/10.1099/jmm.0.001462
Assembly, W. H. (2015). Global Action Plan on Antimicrobial Resistance. Geneva: World Health Organization
Aurilio, C., Sansone, P., Barbarisi, M., Pota, V., Giaccari, L. G., Coppolino, F., Barbarisi, A., Passavanti, M. B., & Pace, M. C. (2022). Mechanisms of Action of Carbapenem Resistance. Antibiotics (Basel, Switzerland), 11(3), 421. https://doi.org/10.3390/antibiotics11030421
Baek, J. Y., Cho, S. Y., Kim, S. H., Kang, C. I., Peck, K. R., Song, J. H., Chung, D. R., & Ko, K. S. (2019). Plasmid analysis of Escherichia coli isolates from South Korea co-producing NDM-5 and OXA-181 carbapenemases. Plasmid, 104, 102417. https://doi.org/10.1016/j.plasmid.2019.102417
Balm, M. N., Ngan, G., Jureen, R., Lin, R. T., & Teo, J. (2012). Molecular characterization of newly emerged blaKPC-2-producing Klebsiella pneumoniae in Singapore. Journalofclinicalmicrobiology, 50(2), 475–476. https://doi.org/10.1128/JCM.05914-11
Barría-Loaiza, C., Pincheira, A., Quezada, M., Vera, A., Valenzuela, P., Domínguez, M., Lima, C. A., Araya, I., Araya, P., Prat, S., Aguayo, C., Fernández, J., Hormazábal, J. C., Bello-Toledo, H., & González-Rocha, G. (2016). Molecular typing and genetic environment of the blaKPC gene in Chilean isolates of Klebsiella pneumoniae. Journal of global antimicrobial resistance, 4, 28–34. https://doi.org/10.1016/j.jgar.2016.01.001
Bell, J. M., Gottlieb, T., Daley, D. A., & Coombs, G. W. (2019). Australian Group on Antimicrobial Resistance (AGAR) Australian Gram-negative Sepsis Outcome Programme (GNSOP) Annual Report 2017. Communicable diseases intelligence (2018), 43, 10.33321/cdi.2019.43.37. https://doi.org/10.33321/cdi.2019.43.37
Bonomo, R. A., Burd, E. M., Conly, J., Limbago, B. M., Poirel, L., Segre, J. A., &Westblade, L. F. (2018). Carbapenemase-Producing Organisms: A Global Scourge. Clinical infectious diseases, 66(8), 1290–1297. https://doi.org/10.1093/cid/cix893
Botelho, J., Mourão, J., Roberts, A. P., &Peixe, L. (2020). Comprehensive genome data analysis establishes a triple whammy of carbapenemases, ICEs and multiple clinically relevant bacteria. Microbial Genomics, 6(10), mgen000424. https://doi.org/10.1099/mgen.0.000424
Bradford, P. A., Bratu, S., Urban, C., Visalli, M., Mariano, N., Landman, D., Rahal, J. J., Brooks, S., Cebular, S., & Quale, J. (2004). Emergence of carbapenem-resistant Klebsiella species possessing the class A carbapenem-hydrolyzing KPC-2 and inhibitor-resistant TEM-30 beta-lactamases in New York City. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America, 39(1), 55–60. https://doi.org/10.1086/421495
Bratu, S., Mooty, M., Nichani, S., Landman, D., Gullans, C., Pettinato, B., Karumudi, U., Tolaney, P., & Quale, J. (2005). Emergence of KPC-possessing Klebsiella pneumoniae in Brooklyn, New York: epidemiology and recommendations for detection. Antimicrobial agents and chemotherapy, 49(7), 3018–3020. https://doi.org/10.1128/AAC.49.7.3018-3020.2005
Bush, K., & Jacoby, G. A. (2010). Updated functional classification of beta-lactamases. Antimicrobialagents and chemotherapy, 54(3), 969–976. https://doi.org/10.1128/AAC.01009-09
Campos, J. C., da Silva, M. J., dos Santos, P. R., Barros, E. M., Pereira, M.deO., Seco, B. M., Magagnin, C. M., Leiroz, L. K., de Oliveira, T. G., de Faria-Júnior, C., Cerdeira, L. T., Barth, A. L., Sampaio, S. C., Zavascki, A. P., Poirel, L., & Sampaio, J. L. (2015). Characterization of Tn3000, a Transposon Responsible for blaNDM-1 Dissemination among Enterobacteriaceae in Brazil, Nepal, Morocco, and India. Antimicrobial agents and chemotherapy, 59(12), 7387–7395. https://doi.org/10.1128/AAC.01458-15
Cantón, R., & Bou, G. (2017). Resistencia antimicrobiana en bacilos gramnegativos: una amenaza actual y global. Enfermedades Infecciosas y Microbiología Clínica, 3-10.
Carvalho-Assef, A. P., Pereira, P. S., Albano, R. M., Berião, G. C., Tavares, C. P., Chagas, T. P., Marques, E. A., Timm, L. N., Da Silva, R. C., Falci, D. R., & Asensi, M. D. (2014). Detection of NDM-1-, CTX-M-15-, and qnrB4-producing Enterobacter hormaechei isolates in Brazil. Antimicrobial agents and chemotherapy, 58(4), 2475–2476. https://doi.org/10.1128/AAC.02804-13
Cerdeira, L. T., Lam, M. M. C., Wyres, K. L., Wick, R. R., Judd, L. M., Lopes, R., Ribas, R. M., Morais, M. M., Holt, K. E., &Lincopan, N. (2019). Small IncQ1 and Col-Like Plasmids Harboring blaKPC-2 and Non-Tn4401 Elements (NTEKPC-IId) in High-Risk Lineages of Klebsiella pneumoniae CG258. Antimicrobial agents and chemotherapy, 63(3), e02140-18. https://doi.org/10.1128/AAC.02140-18
Contreras, D. A., Fitzwater, S. P., Nanayakkara, D. D., Schaenman, J., Aldrovandi, G. M., Garner, O. B., & Yang, S. (2020). Coinfections of Two Strains of NDM-1- and OXA-232-Coproducing Klebsiella pneumoniae in a Kidney Transplant Patient. Antimicrobial agents and chemotherapy, 64(4), e00948-19. https://doi.org/10.1128/AAC.00948-19
Cuzon, G., Naas, T., Truong, H., Villegas, M. V., Wisell, K. T., Carmeli, Y., Gales, A. C., Venezia, S. N., Quinn, J. P., & Nordmann, P. (2010). Worldwide diversity of Klebsiella pneumoniae that produce beta-lactamase blaKPC-2 gene. Emerging infectious diseases, 16(9), 1349–1356. https://doi.org/10.3201/eid1609.091389
De Belder, D., Faccone, D., Tijet, N., Melano, R. G., Rapoport, M., Petroni, A., Lucero, C., Pasteran, F., Corso, A., &Gomez, S. A. (2017). Novel class 1 Integrons and sequence types in VIM-2 and VIM-11-producing clinical strains of Enterobacter cloacae. Infection, genetics and evolution : journal of molecular epidemiology and evolutionary genetics in infectious diseases, 54, 374–378. https://doi.org/10.1016/j.meegid.2017.07.019
Diene, S. M., &Rolain, J. M. (2014). Carbapenemase genes and genetic platforms in Gram-negative bacilli: Enterobacteriaceae, Pseudomonas and Acinetobacter species. Clinical microbiology and infection : the official publication of the European Society of Clinical Microbiology and Infectious Diseases, 20(9), 831–838. https://doi.org/10.1111/1469-0691.12655
Dutescu, I. A., & Hillier, S. A. (2021). Encouraging the Development of New Antibiotics: Are Financial Incentives the Right Way Forward? A Systematic Review and Case Study. Infection and drug resistance, 14, 415–434. https://doi.org/10.2147/IDR.S287792
Drawz, S. M., &Bonomo, R. A. (2010). Three decades of beta-lactamase inhibitors. Clinical microbiology reviews, 23(1), 160–201. https://doi.org/10.1128/CMR.00037-09
Elena, A., Cejas, D., Magariños, F., Jewtuchowicz, V., Facente, A., Gutkind, G., Di Conza, J., &Radice, M. (2018). Spread of Clonally Related Escherichia coli Strains Harboring an IncA/C1 Plasmid Encoding IMP-8 and Its Recruitment into an Unrelated MCR-1-Containing Isolate. Antimicrobialagents and chemotherapy, 62(6), e02414-17. https://doi.org/10.1128/AAC.02414-17
Escobar Pérez, J. A., Olarte Escobar, N. M., Castro-Cardozo, B., Valderrama Márquez, I. A., Garzón Aguilar, M. I., Martinez de la Barrera, L., Barrero Barreto, E. R., Marquez-Ortiz, R. A., Moncada Guayazán, M. V., & Vanegas Gómez, N. (2013). Outbreak of NDM-1-producing Klebsiella pneumoniae in a neonatal unit in Colombia. Antimicrobial agents and chemotherapy, 57(4), 1957–1960. https://doi.org/10.1128/AAC.01447-12
Galetti, R., Andrade, L. N., Varani, A. M., &Darini, A. L. C. (2019). A Phage-Like Plasmid Carrying blaKPC-2 Gene in Carbapenem-Resistant Pseudomonas aeruginosa. Frontiers in microbiology, 10, 572. https://doi.org/10.3389/fmicb.2019.00572
Giddins, M. J., Macesic, N., Annavajhala, M. K., Stump, S., Khan, S., McConville, T. H., Mehta, M., Gomez-Simmonds, A., &Uhlemann, A. C. (2018). Successive Emergence of Ceftazidime-Avibactam Resistance through Distinct Genomic Adaptations in blaKPC-2-Harboring Klebsiella pneumoniae Sequence Type 307 Isolates. Antimicrobial agents and chemotherapy, 62(3), e02101-17. https://doi.org/10.1128/AAC.02101-17
Giske C. G. (2015). Contemporary resistance trends and mechanisms for the old antibiotics colistin, temocillin, fosfomycin, mecillinam and nitrofurantoin. Clinical microbiology and infection : the official publication of the European Society of Clinical Microbiology and Infectious Diseases, 21(10), 899–905. https://doi.org/10.1016/j.cmi.2015.05.022
Godeux, A. S., Svedholm, E., Barreto, S., Potron, A., Venner, S., Charpentier, X., &Laaberki, M. H. (2022). Interbacterial Transfer of Carbapenem Resistance and Large Antibiotic Resistance Islands by Natural Transformation in Pathogenic Acinetobacter. mBio, 13(1), e0263121. https://doi.org/10.1128/mbio.02631-21
Gomez, S. A., Pasteran, F. G., Faccone, D., Tijet, N., Rapoport, M., Lucero, C., Lastovetska, O., Albornoz, E., Galas, M., KPC Group, Melano, R. G., Corso, A., &Petroni, A. (2011). Clonal dissemination of Klebsiella pneumoniae ST258 harbouring KPC-2 in Argentina. Clinical microbiology and infection : the official publication of the European Society of Clinical Microbiology and Infectious Diseases, 17(10), 1520–1524. https://doi.org/10.1111/j.1469-0691.2011.03600.x
Gomez, S., Pasteran, F., Faccone, D., Bettiol, M., Veliz, O., De Belder, D., Rapoport, M., Gatti, B., Petroni, A., &Corso, A. (2013). Intrapatient emergence of OXA-247: a novel carbapenemase found in a patient previously infected with OXA-163-producing Klebsiella pneumoniae. Clinical microbiology and infection : the official publication of the European Society of Clinical Microbiology and Infectious Diseases, 19(5), E233–E235. https://doi.org/10.1111/1469-0691.12142
HammoudiHalat, D., & Ayoub Moubareck, C. (2020). The Current Burden of Carbapenemases: Review of Significant Properties and Dissemination among Gram-Negative Bacteria. Antibiotics (Basel, Switzerland), 9(4), 186. https://doi.org/10.3390/antibiotics9040186
Hansen G. T. (2021). Continuous Evolution: Perspective on the Epidemiology of Carbapenemase Resistance Among Enterobacterales and Other Gram-Negative Bacteria. Infectious Diseases and Therapy, 10(1), 75–92. https://doi.org/10.1007/s40121-020-00395-2
Hellinger, W. C., & Brewer, N. S. (1999). Carbapenems and monobactams: imipenem, meropenem, and aztreonam. Mayo Clinic proceedings, 74(4), 420–434. https://doi.org/10.4065/74.4.420
High Dose Tigecycline for the Treatment of Severe Infections: A Systematic Review and Meta-Analysis. Advances in therapy, 37(3), 1049–1064. https://doi.org/10.1007/s12325-020-01235-y
Ho, C. S., Wong, C. T. H., Aung, T. T., Lakshminarayanan, R., Mehta, J. S., Rauz, S., McNally, A., Kintses, B., Peacock, S. J., de la Fuente-Nunez, C., Hancock, R. E. W., & Ting, D. S. J. (2025). Antimicrobial resistance: a concise update. The Lancet. Microbe, 6(1), 100947. https://doi.org/10.1016/j.lanmic.2024.07.010
Hu, Y. Y., Wang, Q., Sun, Q. L., Chen, G. X., & Zhang, R. (2019). A novel plasmid carrying carbapenem-resistant gene blaKPC-2 in Pseudomonas aeruginosa. Infection and drug resistance, 12, 1285–1288. https://doi.org/10.2147/IDR.S196390
Ji, J., Zhu, Y., Zhao, F., Zhang, J., Yao, B., Zhu, M., Yu, Y., Zhang, J., & Fu, Y. (2024). Co-colonization of different species harboring KPC or NDM carbapenemase in the same host gut: insight of resistance evolution by horizontal gene transfer. Frontiers in Microbiology, 15, 1416454. https://doi.org/10.3389/fmicb.2024.1416454
Kaase, M., Nordmann, P., Wichelhaus, T. A., Gatermann, S. G., Bonnin, R. A., &Poirel, L. (2011). NDM-2 carbapenemase in Acinetobacter baumannii from Egypt. The Journal of antimicrobial chemotherapy, 66(6), 1260–1262. https://doi.org/10.1093/jac/dkr135
Kumarasamy, K., &Kalyanasundaram, A. (2012). Emergence of Klebsiella pneumoniae isolate co-producing NDM-1 with KPC-2 from India. The Journal of antimicrobial chemotherapy, 67(1), 243–244. https://doi.org/10.1093/jac/dkr431
Lauretti, L., Riccio, M. L., Mazzariol, A., Cornaglia, G., Amicosante, G., Fontana, R., &Rossolini, G. M. (1999). Cloning and characterization of blaVIM, a new integron-borne metallo-beta-lactamase gene from a Pseudomonas aeruginosa clinical isolate. Antimicrobial agents and chemotherapy, 43(7), 1584–1590. https://doi.org/10.1128/AAC.43.7.1584
Limbago, B. M., Rasheed, J. K., Anderson, K. F., Zhu, W., Kitchel, B., Watz, N., Munro, S., Gans, H., Banaei, N., & Kallen, A. J. (2011). IMP-producing carbapenem-resistant Klebsiella pneumoniae in the United States. Journal of clinical microbiology, 49(12), 4239–4245. https://doi.org/10.1128/JCM.05297-11
Lincopan, N., McCulloch, J. A., Reinert, C., Cassettari, V. C., Gales, A. C., &Mamizuka, E. M. (2005). First isolation of metallo-beta-lactamase-producing multiresistant Klebsiella pneumoniae from a patient in Brazil. Journal of clinical microbiology, 43(1), 516–519. https://doi.org/10.1128/JCM.43.1.516-519.2005
Logan, L. K., & Weinstein, R. A. (2017). The Epidemiology of Carbapenem-Resistant Enterobacteriaceae: The Impact and Evolution of a Global Menace. The Journal of infectious diseases, 215(suppl_1), S28–S36. https://doi.org/10.1093/infdis/jiw282
Ma, J., Song, X., Li, M., Yu, Z., Cheng, W., Yu, Z., Zhang, W., Zhang, Y., Shen, A., Sun, H., & Li, L. (2023). Global spread of carbapenem-resistant Enterobacteriaceae: Epidemiological features, resistance mechanisms, detection and therapy. Microbiological research, 266, 127249. https://doi.org/10.1016/j.micres.2022.127249
Martin, A., Fahrbach, K., Zhao, Q., &Lodise, T. (2018). Association Between Carbapenem Resistance and Mortality Among Adult, Hospitalized Patients With Serious Infections Due to Enterobacteriaceae: Results of a Systematic Literature Review and Meta-analysis. Open Forum Infectious Diseases, 5(7), ofy150. https://doi.org/10.1093/ofid/ofy150
Massova, I., &Mobashery, S. (1998). Kinship and diversification of bacterial penicillin-binding proteins and beta-lactamases. Antimicrobial agents and chemotherapy, 42(1), 1–17. https://doi.org/10.1128/AAC.42.1.1
Matsumura, Y., Peirano, G., Devinney, R., Bradford, P. A., Motyl, M. R., Adams, M. D., Chen, L., Kreiswirth, B., &Pitout, J. D. D. (2017). Genomic epidemiology of global VIM-producing Enterobacteriaceae. The Journal of antimicrobial chemotherapy, 72(8), 2249–2258. https://doi.org/10.1093/jac/dkx148
McCarthy, K. L., Jennison, A., Wailan, A. M., & Paterson, D. L. (2017). Draft Genome Sequence of an IMP-7-Producing Pseudomonas aeruginosa Bloodstream Infection Isolate from Australia. Genome announcements, 5(27), e00596-17. https://doi.org/10.1128/genomeA.00596-17
McInnes, R. S., McCallum, G. E., Lamberte, L. E., & van Schaik, W. (2020). Horizontal transfer of antibiotic resistance genes in the human gut microbiome. Current Opinion in Microbiology, 53, 35–43. https://doi.org/10.1016/j.mib.2020.02.002
Mojica, M. F., Correa, A., Vargas, D. A., Maya, J. J., Montealegre, M. C., Rojas, L. J., Ruiz, S. J., Quinn, J. P., Villegas, M. V., & Colombian Nosocomial Bacterial Resistance Study Group (2012). Molecular correlates of the spread of KPC-producing Enterobacteriaceae in Colombia. International journal of antimicrobial agents, 40(3), 277–279. https://doi.org/10.1016/j.ijantimicag.2012.05.006
Munkholm, L., & Rubin, O. (2020). The global governance of antimicrobial resistance: a cross-country study of alignment between the global action plan and national action plans. Globalization and health, 16(1), 109. https://doi.org/10.1186/s12992-020-00639-3
Mushi, M. F., Mshana, S. E., Imirzalioglu, C., &Bwanga, F. (2014). Carbapenemase genes among multidrug resistant gram negative clinical isolates from a tertiary hospital in Mwanza, Tanzania. BioMed research international, 2014, 303104. https://doi.org/10.1155/2014/303104
Naas, T., Cuzon, G., Villegas, M. V., Lartigue, M. F., Quinn, J. P., & Nordmann, P. (2008). Genetic structures at the origin of acquisition of the beta-lactamase bla KPC gene. Antimicrobial agents and chemotherapy, 52(4), 1257–1263. https://doi.org/10.1128/AAC.01451-07
Nordmann, P., Naas, T., &Poirel, L. (2011). Global spread of Carbapenemase-producing Enterobacteriaceae. Emerging infectious diseases, 17(10), 1791–1798. https://doi.org/10.3201/eid1710.110655
Nordmann, P., &Poirel, L. (2014). The difficult-to-control spread of carbapenemase producers among Enterobacteriaceae worldwide. Clinical microbiology and infection: the official publication of the European Society of Clinical Microbiology and Infectious Diseases, 20(9), 821–830. https://doi.org/10.1111/1469-0691.12719
Nordmann P. &Poirel L. (2019). Epidemiology and Diagnostics of Carbapenem Resistance in Gram-negative Bacteria. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America, 69(Suppl 7), S521–S528. https://doi.org/10.1093/cid/ciz824
Pasteran, F., Meo, A., Gomez, S., Derdoy, L., Albronoz, E., Faccone, D., Guerriero, L., Archuby, D., Tarzia, A., López, M., &Corso, A. (2014). Emergence of genetically related NDM-1-producing Providencia rettgeri strains in Argentina. Journal of global antimicrobial resistance, 2(4), 344–345. https://doi.org/10.1016/j.jgar.2014.07.003
Pitout, J. D. D., Peirano, G., Kock, M. M., Strydom, K. A., & Matsumura, Y. (2019). The Global Ascendency of OXA-48-Type Carbapenemases. Clinical microbiology reviews, 33(1), e00102-19. https://doi.org/10.1128/CMR.00102-19
Poirel, L., Naas, T., Nicolas, D., Collet, L., Bellais, S., Cavallo, J. D., & Nordmann, P. (2000). Characterization of VIM-2, a carbapenem-hydrolyzing metallo-beta-lactamase and its plasmid- and integron-borne gene from a Pseudomonas aeruginosa clinical isolate in France. Antimicrobial agents and chemotherapy, 44(4), 891–897. https://doi.org/10.1128/AAC.44.4.891-897.2000
Poirel, L., Héritier, C., Tolün, V., & Nordmann, P. (2004). Emergence of oxacillinase-mediated resistance to imipenem in Klebsiella pneumoniae. Antimicrobial agents and chemotherapy, 48(1), 15–22. https://doi.org/10.1128/AAC.48.1.15-22.2004
Poirel, L., Abdelaziz, M. O., Bernabeu, S., & Nordmann, P. (2013). Occurrence of OXA-48 and VIM-1 carbapenemase-producing Enterobacteriaceae in Egypt. International journal of antimicrobial agents, 41(1), 90–91. https://doi.org/10.1016/j.ijantimicag.2012.08.015
Poirel, L., Bonnin, R. A., & Nordmann, P. (2012). Genetic features of the widespread plasmid coding for the carbapenemase OXA-48. Antimicrobial agents and chemotherapy, 56(1), 559–562. https://doi.org/10.1128/AAC.05289-11
Qin, X., Ding, L., Hao, M., Li, P., Hu, F., & Wang, M. (2024). Antimicrobial resistance of clinical bacterial isolates in China: current status and trends. JAC-antimicrobial resistance, 6(2), dlae052. https://doi.org/10.1093/jacamr/dlae052
Queenan, A. M., & Bush, K. (2007). Carbapenemases: the versatile beta-lactamases. Clinical microbiology reviews, 20(3), 440–458. https://doi.org/10.1128/CMR.00001-07
Reyes, J. A., Villavicencio, F., Villacís, J. E., Pavón, E., Campoverde, N., Espinel, M., Núñez, B., & Trueba, G. (2020). First report of a clinical isolate of blaOXA-48- carbapenemase producing Raoultellaornithinolytica in South America. Revista Argentina de microbiologia, 52(1), 82–83. https://doi.org/10.1016/j.ram.2019.02.002
Riccio, M. L., Franceschini, N., Boschi, L., Caravelli, B., Cornaglia, G., Fontana, R., Amicosante, G., &Rossolini, G. M. (2000). Characterization of the metallo-beta-lactamase determinant of Acinetobacter baumannii AC-54/97 reveals the existence of bla(IMP) allelic variants carried by gene cassettes of different phylogeny. Antimicrobial agents and chemotherapy, 44(5), 1229–1235. https://doi.org/10.1128/AAC.44.5.1229-1235.2000
Rocha, C., Reynolds, N. D., & Simons, M. P. (2015). Resistencia emergente a los antibióticos: una amenaza global y un problema crítico en el cuidado de la salud. Revista Peruana De Medicina Experimental Y Salud Pública, 32(1), 139-145.
Rojas, L. J., Wright, M. S., De La Cadena, E., Motoa, G., Hujer, K. M., Villegas, M. V., Adams, M. D., &Bonomo, R. A. (2016). Initial Assessment of the Molecular Epidemiology of blaNDM-1 in Colombia. Antimicrobialagents and chemotherapy, 60(7), 4346–4350. https://doi.org/10.1128/AAC.03072-15
Salam, M. A., Al-Amin, M. Y., Salam, M. T., Pawar, J. S., Akhter, N., Rabaan, A. A., &Alqumber, M. A. A. (2023). Antimicrobial Resistance: A Growing Serious Threat for Global Public Health. Healthcare (Basel, Switzerland), 11(13), 1946. https://doi.org/10.3390/healthcare11131946
Silva, K. E., Cayô, R., Carvalhaes, C. G., Patussi Correia Sacchi, F., Rodrigues-Costa, F., Ramos da Silva, A. C., Croda, J., Gales, A. C., &Simionatto, S. (2015). Coproduction of KPC-2 and IMP-10 in Carbapenem-Resistant Serratia marcescens Isolates from an Outbreak in a Brazilian Teaching Hospital. Journal of clinical microbiology, 53(7), 2324–2328. https://doi.org/10.1128/JCM.00727-15
Solgi, H., Badmasti, F., Aminzadeh, Z., Giske, C. G., Pourahmad, M., Vaziri, F., Havaei, S. A., &Shahcheraghi, F. (2017). Molecular characterization of intestinal carriage of carbapenem-resistant Enterobacteriaceae among inpatients at two Iranian university hospitals: first report of co-production of bla NDM-7 and bla OXA-48. European journal of clinical microbiology & infectious diseases, 36(11), 2127–2135. https://doi.org/10.1007/s10096-017-3035-3
Stewart, A., Harris, P., Henderson, A., & Paterson, D. (2018). Treatment of Infections by OXA-48-Producing Enterobacteriaceae. Antimicrobial agents and chemotherapy, 62(11), e01195-18. https://doi.org/10.1128/AAC.01195-18
Tavares, C. P., Pereira, P. S., Marques, E.deA., Faria, C., Jr, de Souza, M.daP., de Almeida, R., Alves, C.deF., Asensi, M. D., & Carvalho-Assef, A. P. (2015). Molecular epidemiology of KPC-2-producing Enterobacteriaceae (non-Klebsiella pneumoniae) isolated from Brazil. Diagnostic microbiology and infectious disease, 82(4), 326–330. https://doi.org/10.1016/j.diagmicrobio.2015.04.002
Temkin, E., Fallach, N., Almagor, J., Gladstone, B. P., Tacconelli, E., Carmeli, Y., & DRIVE-AB Consortium (2018). Estimating the number of infections caused by antibiotic-resistant Escherichia coli and Klebsiella pneumoniae in 2014: a modelling study. The Lancet. Global health, 6(9), e969–e979. https://doi.org/10.1016/S2214-109X(18)30278-X
Tenover, F. C., Nicolau, D. P., & Gill, C. M. (2022). Carbapenemase-producing Pseudomonas aeruginosa -an emerging challenge. Emerging Microbes & Infections, 11(1), 811–814. https://doi.org/10.1080/22221751.2022.2048972
Toleman, M. A., Rolston, K., Jones, R. N., & Walsh, T. R. (2004). blaVIM-7, an evolutionarily distinct metallo-beta-lactamase gene in a Pseudomonas aeruginosa isolate from the United States. Antimicrobial agents and chemotherapy, 48(1), 329–332. https://doi.org/10.1128/AAC.48.1.329-332.2004
Turton, J. F., Doumith, M., Hopkins, K. L., Perry, C., Meunier, D., & Woodford, N. (2016). Clonal expansion of Escherichia coli ST38 carrying a chromosomally integrated OXA-48 carbapenemase gene. Journal of medical microbiology, 65(6), 538–546. https://doi.org/10.1099/jmm.0.000248
UK Health Security Agency English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) Report 2022 to 2023. 2023. Available online: https://webarchive.nationalarchives.gov.uk/ukgwa/20240127185100mp_/https://assets.
publishing.service.gov.uk/media/6555026e544aea000dfb2e19/ESPAUR-report-2022-to-2023.pdf
van Beek, J., Räisänen, K., Broas, M., Kauranen, J., Kähkölä, A., Laine, J., Mustonen, E., Nurkkala, T., Puhto, T., Sinkkonen, J., Torvinen, S., Vornanen, T., Vuento, R., Jalava, J., &Lyytikäinen, O. (2019). Tracing local and regional clusters of carbapenemase-producing Klebsiella pneumoniae ST512 with whole genome sequencing, Finland, 2013 to 2018. Euro surveillance : bulletin Europeen sur les maladies transmissibles = European communicable disease bulletin, 24(38), 1800522. https://doi.org/10.2807/1560-7917.ES.2019.24.38.1800522
van Duin, D., & Doi, Y. (2017). The global epidemiology of carbapenemase-producing Enterobacteriaceae. Virulence, 8(4), 460–469. https://doi.org/10.1080/21505594.2016.1222343
Wailan, A. M., Paterson, D. L., Kennedy, K., Ingram, P. R., Bursle, E., &Sidjabat, H. E. (2015). Genomic Characteristics of NDM-Producing Enterobacteriaceae Isolates in Australia and Their blaNDM Genetic Contexts. Antimicrobial agents and chemotherapy, 60(1), 136–141. https://doi.org/10.1128/AAC.01243-15
Watanabe, M., Iyobe, S., Inoue, M., & Mitsuhashi, S. (1991). Transferableimipenemresistance in Pseudomonas aeruginosa. Antimicrobial agents and chemotherapy, 35(1), 147–151. https://doi.org/10.1128/AAC.35.1.147
Wise, M. G., Karlowsky, J. A., Mohamed, N., Hermsen, E. D., Kamat, S., Townsend, A., Brink, A., Soriano, A., Paterson, D. L., Moore, L. S. P., &Sahm, D. F. (2024). Global trends in carbapenem- and difficult-to-treat-resistance among World Health Organization priority bacterial pathogens: ATLAS surveillance program 2018-2022. Journal of global antimicrobial resistance, 37, 168–175. https://doi.org/10.1016/j.jgar.2024.03.020
Woodford, N., Tierno, P. M., Jr, Young, K., Tysall, L., Palepou, M. F., Ward, E., Painter, R. E., Suber, D. F., Shungu, D., Silver, L. L., Inglima, K., Kornblum, J., & Livermore, D. M. (2004). Outbreak of Klebsiella pneumoniae producing a new carbapenem-hydrolyzing class A beta-lactamase, KPC-3, in a New York Medical Center. Antimicrobial agents and chemotherapy, 48(12), 4793–4799. https://doi.org/10.1128/AAC.48.12.4793-4799.2004
World Health Organization. (2019). 2019 antibacterial agents in clinical development: An analysis of the antibacterial clinical development pipeline. World Health Organization. https://www.who.int/publications-detail-redirect/9789240000193
Yigit, H., Queenan, A. M., Anderson, G. J., Domenech-Sanchez, A., Biddle, J. W., Steward, C. D., Alberti, S., Bush, K., &Tenover, F. C. (2001). Novel carbapenem-hydrolyzing beta-lactamase, KPC-1, from a carbapenem-resistant strain of Klebsiella pneumoniae. Antimicrobial agents and chemotherapy, 45(4), 1151–1161. https://doi.org/10.1128/AAC.45.4.1151-1161.2001
Yong, D., Toleman, M. A., Giske, C. G., Cho, H. S., Sundman, K., Lee, K., & Walsh, T. R. (2009). Characterization of a new metallo-beta-lactamase gene, bla(NDM-1), and a novel erythromycin esterase gene carried on a unique genetic structure in Klebsiella pneumoniae sequence type 14 from India. Antimicrobial agents and chemotherapy, 53(12), 5046–5054. https://doi.org/10.1128/AAC.00774-09
Yuan, P.-B., Dai, L.-T., Zhang, Q.-K., Zhong, Y.-X., Liu, W.-T., Yang, L., & Chen, D.-Q. (2024). Global emergence of double and multi-carbapenemase producing organisms: epidemiology, clinical significance, and evolutionary benefits on antimicrobial resistance and virulence. Microbiology spectrum, 12(7), e0000824. https://doi.org/10.1128/spectrum.00008-24
Zha, L., Pan, L., Guo, J., French, N., Villanueva, E. V., &Tefsen, B. (2020). Effectiveness and Safety of High Dose Tigecycline for the Treatment of Severe Infections: A Systematic Review and Meta-Analysis. Advances in therapy, 37(3), 1049–1064. https://doi.org/10.1007/s12325-020-01235-y
Zhanel, G. G., Simor, A. E., Vercaigne, L., Mandell, L., & Canadian Carbapenem Discussion Group (1998). Imipenem and meropenem: Comparison of in vitro activity, pharmacokinetics, clinical trials and adverse effects. The Canadian journal of infectious diseases = Journal canadien des maladies infectieuses, 9(4), 215–228. https://doi.org/10.1155/1998/831425
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Revista Geográfica de Chile Terra Australis

This work is licensed under a Creative Commons Attribution 4.0 International License.
Copyright notice:
Revista Geográfica de Chile Terra Australis retains the economic rights (copyright) of the works published in the Revista Geográfica de Chile Terra Australis. The reuse of the content is allowed under a license:
CC BY
Recognition

This license allows others to distribute, remix, tweak and build upon your work, even for commercial purposes, as long as you are acknowledged as the author of the original creation. This is the most helpful license offered. It is recommended for maximum dissemination and use of the materials subject to the license.