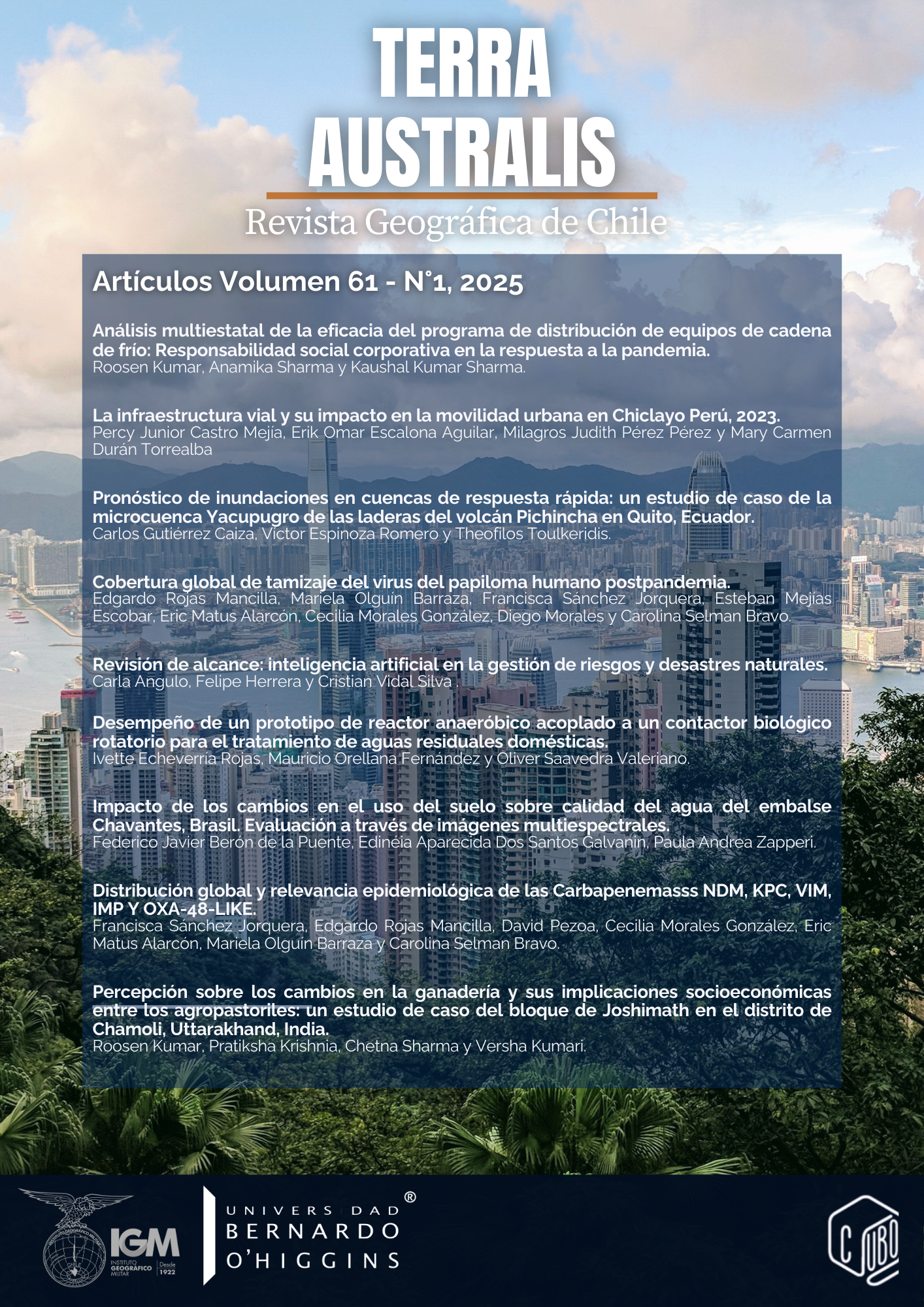
Post-pandemic global coverage of human papillomavirus screening
DOI:
https://doi.org/10.23854/07199562.2025611.mancillaKeywords:
Virus del Papiloma Humano (VPH), cáncer cervicouterino, tamizaje, COVID-19Abstract
Human papillomavirus (HPV) is the leading cause of cervical cancer, one of the main causes of female mortality worldwide. Early detection through screening programs, including HPV testing and cytology, is crucial to prevent progression to invasive cancer and reduce mortality. However, the coverage of these programs presents marked geographic disparities, reflecting inequalities in access and resources. Before the COVID-19 pandemic, screening coverage was already insufficient, especially in low- and middle-income countries, where rates were significantly lower than in high-income countries. The pandemic exacerbated this problem, generating a significant reduction in screening coverage during pandemic. The impact after the health emergency has been analyzed in this review. The decline in coverage has not recovered to pre-pandemic levels, representing a relevant threat to public health, especially among the most vulnerable populations. The data showed a clear correlation between a country's income level and its ability to maintain adequate cervical cancer screening coverage. While high-income countries maintain relatively high coverage, low- and middle-income countries continue to face significant access barriers, including limitations in infrastructure, economic resources, access to screening exams and access to trained personnel. Identifying and addressing these inequalities is crucial to designing and implementing effective prevention and control strategies that reduce cervical cancer morbidity and mortality globally. Significant investment is required in health infrastructure, health education programs, and public policies that promote equity in access to quality health services.
Downloads
References
Adcock, R., Cuzick, J., Hunt, W. C., McDonald, R. M., Wheeler, C. M., & New Mexico HPV Pap Registry Steering Committee (2019). Role of HPV Genotype, Multiple Infections, and Viral Load on the Risk of High-Grade Cervical Neoplasia. Cancer Epidemiology, Biomarkers & Prevention, 28(11), 1816–1824. https://doi.org/10.1158/1055-9965.EPI-19-0239
Aden, D., Zaheer, S., & Raj, S. (2022). Challenges faced in the cancer diagnosis and management-COVID-19 pandemic and beyond-Lessons for future. Heliyon, 8(12), e12091. https://doi.org/10.1016/j.heliyon.2022.e12091
Aden, D., Zaheer, S., Khan, S., Jairajpuri, Z. S., &Jetley, S. (2024). Navigating the landscape of HPV-associated cancers: From epidemiology to prevention. Pathology, Research and Practice, 263, 155574. https://doi.org/10.1016/j.prp.2024.155574
Afsah, Y. R., & Kaneko, N. (2023). Barriers to cervical cancer screening faced by immigrant Muslim women: a systematic scoping review. BMC Public Health, 23(1), 2375. https://doi.org/10.1186/s12889-023-17309-9
Aoki, E. S., Yin, R., Li, K., Bhatla, N., Singhal, S., Ocviyanti, D., Saika, K., Suh, M., Kim, M., &Termrungruanglert, W. (2020). National screening programs for cervical cancer in Asian countries. Journal of Gynecologic Oncology, 31(3), e55. https://doi.org/10.3802/jgo.2020.31.e55
Bogdanova, A., Andrawos, C., &Constantinou, C. (2022). Cervical cancer, geographical inequalities, prevention and barriers in resource depleted countries. Oncology Letters, 23(4), 113. https://doi.org/10.3892/ol.2022.13233
Bouvard, V., Wentzensen, N., Mackie, A., Berkhof, J., Brotherton, J., Giorgi-Rossi, P., Kupets, R., Smith, R., Arrossi, S., Bendahhou, K., Canfell, K., Chirenje, Z. M., Chung, M. H., Del Pino, M., de Sanjosé, S., Elfström, M., Franco, E. L., Hamashima, C., Hamers, F. F., Herrington, C. S., … Lauby-Secretan, B. (2021). The IARC Perspective on Cervical Cancer Screening. The New England Journal of Medicine, 385(20), 1908–1918. https://doi.org/10.1056/NEJMsr2030640
Bruni, L., Serrano, B., Roura, E., Alemany, L., Cowan, M., Herrero, R., Poljak, M., Murillo, R., Broutet, N., Riley, L. M., & de Sanjose, S. (2022). Cervical cancer screening programmes and age-specific coverage estimates for 202 countries and territories worldwide: a review and synthetic analysis. The Lancet. Global Health, 10(8), e1115–e1127. https://doi.org/10.1016/S2214-109X(22)00241-8
Buskwofie, A., David-West, G., & Clare, C. A. (2020). A Review of Cervical Cancer: Incidence and Disparities. Journal of the National Medical Association, 112(2), 229–232. https://doi.org/10.1016/j.jnma.2020.03.002
Canfell, K., Kim, J. J., Brisson, M., Keane, A., Simms, K. T., Caruana, M., Burger, E. A., Martin, D., Nguyen, D. T. N., Bénard, É., Sy, S., Regan, C., Drolet, M., Gingras, G., Laprise, J. F., Torode, J., Smith, M. A., Fidarova, E., Trapani, D., Bray, F., … Hutubessy, R. (2020). Mortality impact of achieving WHO cervical cancer elimination targets: a comparative modelling analysis in 78 low-income and lower-middle-income countries. Lancet (London, England), 395(10224), 591–603. https://doi.org/10.1016/S0140-6736(20)30157-4
Cuzick, J., Clavel, C., Petry, K. U., Meijer, C. J., Hoyer, H., Ratnam, S., Szarewski, A., Birembaut, P., Kulasingam, S., Sasieni, P., &Iftner, T. (2006). Overview of the European and North American studies on HPV testing in primary cervical cancer screening. International Journal of Cancer, 119(5), 1095–1101. https://doi.org/10.1002/ijc.21955
Descamps, P., Bosch Jose, F. X., Monsonego, J., Neisingh, O., Nguyen, L., & O'Connor, M. (2025). Cervical cancer screening: Sharing best practices and addressing common challenges in cervical cancer screening programs. International journal of cancer, 156(3), 679–681. https://doi.org/10.1002/ijc.35220
Elfström KM, Dillner J. Cervical cancer screening improvements with self-sampling during the COVID-19 pandemic [Internet]. MedRxiv. 2022 [cited 2022 Dec 21]. p. 2022.07.19.22277806. Available from: https://www.medrxiv.org/content/10.1101/2022.07.19.22277806v1
Fernández-Deaza, G., Serrano, B., Roura, E., Castillo, J. S., Caicedo-Martínez, M., Bruni, L., & Murillo, R. (2024). Cervical cancer screening coverage in the Americas region: a synthetic analysis. Lancet Regional Health. Americas, 30, 100689. https://doi.org/10.1016/j.lana.2024.100689
Filho, A. M., Laversanne, M., Ferlay, J., Colombet, M., Piñeros, M., Znaor, A., Parkin, D. M., Soerjomataram, I., & Bray, F. (2025). The GLOBOCAN 2022 cancer estimates: Data sources, methods, and a snapshot of the cancer burden worldwide. International Journal of Cancer, 156(7), 1336–1346. https://doi.org/10.1002/ijc.35278
Gakidou, E., Nordhagen, S., & Obermeyer, Z. (2008). Coverage of cervical cancer screening in 57 countries: low average levels and large inequalities. PLoS Medicine, 5(6), e132. https://doi.org/10.1371/journal.pmed.0050132
Gerstl, S., Lee, L., Nesbitt, R. C., Mambula, C., Sugianto, H., Phiri, T., Kachingwe, J., & Llosa, A. E. (2022). Cervical cancer screening coverage and its related knowledge in southern Malawi. BMC public health, 22(1), 295. https://doi.org/10.1186/s12889-022-12547-9
Gopalkrishnan, K., & Karim, R. (2025). Addressing Global Disparities in Cervical Cancer Burden: A Narrative Review of Emerging Strategies. Current HIV/AIDS Reports, 22(1), 18. https://doi.org/10.1007/s11904-025-00727-2
Gourd E. (2021). COVID-19 pandemic causes cervical cancer screening crisis. The Lancet. Oncology, 22(8), 1060. https://doi.org/10.1016/S1470-2045(21)00382-X
Islam, R. M., Billah, B., Hossain, M. N., &Oldroyd, J. (2017). Barriers to Cervical Cancer and Breast Cancer Screening Uptake in Low-Income and Middle-Income Countries: A Systematic Review. Asian Pacific Journal of Cancer Prevention : APJCP, 18(7), 1751–1763. https://doi.org/10.22034/APJCP.2017.18.7.1751
Jensen, J. E., Becker, G. L., Jackson, J. B., &Rysavy, M. B. (2024). Human Papillomavirus and Associated Cancers: A Review. Viruses, 16(5), 680. https://doi.org/10.3390/v16050680
Kessler T. A. (2017). Cervical Cancer: Prevention and Early Detection. Seminars in Oncology Nursing, 33(2), 172–183. https://doi.org/10.1016/j.soncn.2017.02.005
Kundrod, K. A., Jeronimo, J., Vetter, B., Maza, M., Murenzi, G., Phoolcharoen, N., & Castle, P. E. (2023). Toward 70% cervical cancer screening coverage: Technical challenges and opportunities to increase access to human papillomavirus (HPV) testing. PLOS Global Public Health, 3(8), e0001982. https://doi.org/10.1371/journal.pgph.0001982
Lofters, A. K., Wu, F., Frymire, E., Kiran, T., Vahabi, M., Green, M. E., & Glazier, R. H. (2023). Cancer Screening Disparities Before and After the COVID-19 Pandemic. JAMA network open, 6(11), e2343796. https://doi.org/10.1001/jamanetworkopen.2023.43796
Lott, B. E., Trejo, M. J., Baum, C., McClelland, D. J., Adsul, P., Madhivanan, P., Carvajal, S., Ernst, K., &Ehiri, J. (2020). Interventions to increase uptake of cervical screening in sub-Saharan Africa: a scoping review using the integrated behavioral model. BMC Public Health, 20(1), 654. https://doi.org/10.1186/s12889-020-08777-4
Machii, R., Takahashi, H., Miyazawa, J., & Nakayama, T. (2024). Cancer screening in Japan 2 years after the COVID-19 pandemic: Changes in participation, 2017-2021. Preventive Medicine Reports, 39, 102649. https://doi.org/10.1016/j.pmedr.2024.102649
Olusola, P., Banerjee, H. N., Philley, J. V., & Dasgupta, S. (2019). Human Papilloma Virus-Associated Cervical Cancer and Health Disparities. Cells, 8(6), 622. https://doi.org/10.3390/cells8060622
Olthof, E. M. G., Aitken, C. A., Siebers, A. G., van Kemenade, F. J., & de Kok, I. M. C. M. (2024). Resilience of the Dutch HPV-based cervical screening programme during the COVID-19 pandemic. Public Health, 227, 42–48. https://doi.org/10.1016/j.puhe.2023.11.026
Ong, S. K., Abe, S. K., Thilagaratnam, S., Haruyama, R., Pathak, R., Jayasekara, H., Togawa, K., Bhandari, A. K. C., Shankar, A., Nessa, A., Jugder, U., Agustina, J., Biglari, M., Yusuf, A., Tshomo, U., Fernando, E., Cairo, C., Kaung, K. K., Rath, B., Vongdala, C., … Hwang, W. Y. K. (2023). Towards elimination of cervical cancer - human papillomavirus (HPV) vaccination and cervical cancer screening in Asian National Cancer Centers Alliance (ANCCA) member countries. The Lancet regional health. Western Pacific, 39, 100860. https://doi.org/10.1016/j.lanwpc.2023.100860
Osmani, V., Hörner, L., Nkurunziza, T., Rank, S., Tanaka, L. F., & Klug, S. J. (2025). Global prevalence of cervical human papillomavirus in women aged 50 years and older with normal cytology: a systematic review and meta-analysis. The Lancet. Microbe, 6(1), 100955. https://doi.org/10.1016/j.lanmic.2024.100955
Perkins, R. B., Wentzensen, N., Guido, R. S., & Schiffman, M. (2023). Cervical Cancer Screening: A Review. JAMA, 330(6), 547–558. https://doi.org/10.1001/jama.2023.13174
Pilleron, S., Cabasag, C. J., Ferlay, J., Bray, F., Luciani, S., Almonte, M., & Piñeros, M. (2020). Cervical cancer burden in Latin America and the Caribbean: Where are we?. International Journal of Cancer, 147(6), 1638–1648. https://doi.org/10.1002/ijc.32956
Portero de la Cruz, S., &Cebrino, J. (2022). Trends and Determinants in Uptake of Cervical Cancer Screening in Spain: An Analysis of National Surveys from 2017 and 2020. Cancers, 14(10), 2481. https://doi.org/10.3390/cancers14102481
Ramírez, A. T., Valls, J., Baena, A., Rojas, F. D., Ramírez, K., Álvarez, R., Cristaldo, C., Henríquez, O., Moreno, A., Reynaga, D. C., Palma, H. G., Robinson, I., Hernández, D. C., Bardales, R., Cardinal, L., Salgado, Y., Martínez, S., González, E., Guillén, D., Fleider, L., … ESTAMPA Study Group (2023). Performance of cervical cytology and HPV testing for primary cervical cancer screening in Latin America: an analysis within the ESTAMPA study. Lancet Regional Health. Americas, 26, 100593. https://doi.org/10.1016/j.lana.2023.100593
Rojas-Zumaran, V., Walttuoni-Picón, E., Campos-Siccha, G., Cruz-Gonzales, G., Huiza-Espinoza, L., & Moya-Salazar, J. (2022). Decline of cytology-based cervical cancer screening for COVID-19: a single-center Peruvian experience. Declive del cribado de cáncer cervical basado en citología by COVID-19: una experiencia unicéntrica peruana. Medwave, 22(10), e2589. https://doi.org/10.5867/medwave.2022.S3.2589
Saslow, D., Solomon, D., Lawson, H. W., Killackey, M., Kulasingam, S. L., Cain, J., Garcia, F. A., Moriarty, A. T., Waxman, A. G., Wilbur, D. C., Wentzensen, N., Downs, L. S., Jr, Spitzer, M., Moscicki, A. B., Franco, E. L., Stoler, M. H., Schiffman, M., Castle, P. E., Myers, E. R., & ACS-ASCCP-ASCP Cervical Cancer Guideline Committee (2012). American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. CA: a cancer Journal for Clinicians, 62(3), 147–172. https://doi.org/10.3322/caac.21139
Schubert, M., Bauerschlag, D. O., Muallem, M. Z., Maass, N., &Alkatout, I. (2023). Challenges in the Diagnosis and Individualized Treatment of Cervical Cancer. Medicina (Kaunas, Lithuania), 59(5), 925. https://doi.org/10.3390/medicina59050925
Serrano, B., Ibáñez, R., Robles, C., Peremiquel-Trillas, P., de Sanjosé, S., & Bruni, L. (2022). Worldwide use of HPV self-sampling for cervical cancer screening. Preventive Medicine, 154, 106900. https://doi.org/10.1016/j.ypmed.2021.106900
Suk, R., Hong, Y. R., Rajan, S. S., Xie, Z., Zhu, Y., & Spencer, J. C. (2022). Assessment of US Preventive Services Task Force Guideline-Concordant Cervical Cancer Screening Rates and Reasons for Underscreening by Age, Race and Ethnicity, Sexual Orientation, Rurality, and Insurance, 2005 to 2019. JAMA Network Open, 5(1), e2143582. https://doi.org/10.1001/jamanetworkopen.2021.43582
Sung, H., Ferlay, J., Siegel, R. L., Laversanne, M., Soerjomataram, I., Jemal, A., & Bray, F. (2021). Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA: a Cancer Journal for Clinicians, 71(3), 209–249. https://doi.org/10.3322/caac.21660
Téguété, I., Tounkara, F. K., Diawara, B., Traoré, S., Koné, D., Bagayogo, A., Sissoko, A., &Traoré, C. B. (2021). A population-based combination strategy to improve the cervical cancer screening coverage rate in Bamako, Mali. Acta obstetricia et gynecologicaScandinavica, 100(4), 794–801. https://doi.org/10.1111/aogs.14119
Teixeira, J. C., Vale, D. B., Campos, C. S., Polegatto, I., Bragança, J. F., Discacciati, M. G., & Zeferino, L. C. (2024). Transition from opportunistic cytological to organized screening program with DNA-HPV testing detected prevalent cervical cancers 10 years in advance. Scientific reports, 14(1), 20761. https://doi.org/10.1038/s41598-024-71735-2
US Preventive Services Task Force, Curry, S. J., Krist, A. H., Owens, D. K., Barry, M. J., Caughey, A. B., Davidson, K. W., Doubeni, C. A., Epling, J. W., Jr, Kemper, A. R., Kubik, M., Landefeld, C. S., Mangione, C. M., Phipps, M. G., Silverstein, M., Simon, M. A., Tseng, C. W., & Wong, J. B. (2018). Screening for Cervical Cancer: US Preventive Services Task Force Recommendation Statement. JAMA, 320(7), 674–686. https://doi.org/10.1001/jama.2018.10897
Wang, M., Maimaitiming, M., Bi, Y., &Jin, Y. (2024). Compliance Rate With Triage Test and Treatment for Participants Screening Positive in Cervical Cancer Screening Programs: A Systematic Review and Meta-analysis. Obstetrics and Gynecology, 144(6), 791–800. https://doi.org/10.1097/AOG.0000000000005723
Wei, F., Georges, D., Man, I., Baussano, I., & Clifford, G. M. (2024). Causal attribution of human papillomavirus genotypes to invasive cervical cancer worldwide: a systematic analysis of the global literature. Lancet, 404(10451), 435–444. https://doi.org/10.1016/S0140-6736(24)01097-3
Wentzensen, N., Clarke, M. A., & Perkins, R. B. (2021). Impact of COVID-19 on cervical cancer screening: Challenges and opportunities to improving resilience and reduce disparities. Preventive Medicine, 151, 106596. https://doi.org/10.1016/j.ypmed.2021.106596
World Health Organization (WHO), Global cancer observatory (GLOBOCAN), International Agency for Research on Cancer (IARC) [Internet]. Data viz. Cancer today. 2022 [cited 2025 Mar 20]. Available from: https://gco.iarc.fr/today/en/dataviz/bars-compare-populations?mode=cancer&key=crude_rate&cancers=15&populations=152&group_populations=1&types=0_1&sort_by=value1&sexes=2
World Health Organization (WHO). (2020). Impact of the COVID-19 pandemic on noncommunicable disease resources and services: Results of a rapid assessment. WHO. Recuperado de: https://www.who.int/publications/i/item/9789240010291
WHO guideline for screening and treatment of cervical pre-cancer lesions for cervical cancer prevention. (2021). (2nd ed.). World Health Organization.
Yimer, N. B., Mohammed, M. A., Solomon, K., Tadese, M., Grutzmacher, S., Meikena, H. K., Alemnew, B., Sharew, N. T., &Habtewold, T. D. (2021). Cervical cancer screening uptake in Sub-Saharan Africa: a systematic review and meta-analysis. Public Health, 195, 105–111. https://doi.org/10.1016/j.puhe.2021.04.014
Zhang, M., Zhong, Y., Wang, L., Bao, H., Huang, Z., Zhao, Z., Zhang, X., Li, C., Sun, K. L., Wu, J., Zheng, X., & Wang, L. (2022). Cervical Cancer Screening Coverage - China, 2018-2019. China CDC weekly, 4(48), 1077–1082. https://doi.org/10.46234/ccdcw2022.217
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Revista Geográfica de Chile Terra Australis

This work is licensed under a Creative Commons Attribution 4.0 International License.
Copyright notice:
Revista Geográfica de Chile Terra Australis retains the economic rights (copyright) of the works published in the Revista Geográfica de Chile Terra Australis. The reuse of the content is allowed under a license:
CC BY
Recognition

This license allows others to distribute, remix, tweak and build upon your work, even for commercial purposes, as long as you are acknowledged as the author of the original creation. This is the most helpful license offered. It is recommended for maximum dissemination and use of the materials subject to the license.